Evaluating and Testing Persons for Coronavirus Disease 2019 (COVID-19)
Related Pages
CDC guidance for COVID-19 may be adapted by state and local health departments to respond to rapidly changing local circumstances.
Summary of Recent Changes
Revisions were made on March 24, 2020 to reflect the following:
Updated priorities for testing patients with suspected COVID-19 infection
Revisions were made on March 9, 2020, to reflect the following:
Reorganized the Criteria to Guide Evaluation and Laboratory Testing for COVID-19 section
Revisions were made on March 4, 2020, to reflect the following:
Criteria for evaluation of persons for testing for COVID-19 were expanded to include a wider group of symptomatic patients.
Updated March 24, 2020
Limited information is available to characterize the spectrum of clinical illness associated with coronavirus disease 2019 (COVID-19). No vaccine or specific treatment for COVID-19 is available; care is supportive.
The CDC clinical criteria for considering testing for COVID-19 have been developed based on what is known about COVID-19 and are subject to change as additional information becomes available.
CDC Health Advisory

Update and Interim Guidance on Outbreak of Coronavirus Disease 2019 (COVID-19)
CDC continues to closely monitor an outbreak of respiratory illness caused by COVID-19 that was initially detected in Wuhan City, Hubei Province, China. This HAN Update provides a situational update and guidance to state and local health departments and health care providers.
phone icon
Contact your local or state health department
Healthcare providers should immediately notify their localexternal icon or stateexternal icon health department in the event of the identification of a PUI for COVID-19. When working with your local or state health department check their available hours.
Criteria to Guide Evaluation and Laboratory Testing for COVID-19
Clinicians considering testing of persons with possible COVID-19 should continue to work with their local and state health departments to coordinate testing through public health laboratories, or use COVID-19 diagnostic testing, authorized by the Food and Drug Administration under an Emergency Use Authorization (EUA) through clinical laboratories. Increasing testing capacity will allow clinicians to consider COVID-19 testing for a wider group of symptomatic patients.
Clinicians should use their judgment to determine if a patient has signs and symptoms compatible with COVID-19 and whether the patient should be tested. Most patients with confirmed COVID-19 have developed fever1 and/or symptoms of acute respiratory illness (e.g., cough, difficulty breathing). Priorities for testing include:
Other considerations that may guide testing are epidemiologic factors such as the occurrence of local community transmission of COVID-19 infections in a jurisdiction. Clinicians are strongly encouraged to test for other causes of respiratory illness.
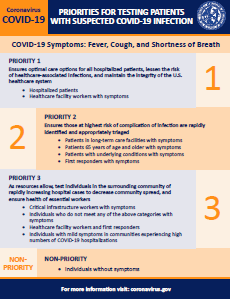
Priorities for testing patients with suspected COVID-19 infection
pdf icon[PDF – 202 KB]
| PRIORITY 1
Ensure optimal care options for all hospitalized patients, lessen the risk of nosocomial infections, and maintain the integrity of the healthcare system Hospitalized patients |
| PRIORITY 2
Ensure that those who are at highest risk of complication of infection are rapidly identified and appropriately triaged Patients in long-term care facilities with symptoms |
| PRIORITY 3
As resources allow, test individuals in the surrounding community of rapidly increasing hospital cases to decrease community spread, and ensure health of essential workers Critical infrastructure workers with symptoms |
| NON-PRIORITY
Individuals without symptoms |
Recommendations for Reporting, Testing, and Specimen Collection
Updated February 28, 2020
Clinicians should immediately implement recommended infection prevention and control practices if a patient is suspected of having COVID-19. They should also notify infection control personnel at their healthcare facility and their state or local health department if a patient is classified as a PUI for COVID-19. State health departments that have identified a PUI or a laboratory-confirmed case should complete a PUI and Case Report form through the processes identified on CDC’s Coronavirus Disease 2019 website. State and local health departments can contact CDC’s Emergency Operations Center (EOC) at 770-488-7100 for assistance with obtaining, storing, and shipping appropriate specimens to CDC for testing, including after hours or on weekends or holidays.
For initial diagnostic testing for COVID-19, CDC recommends collecting and testing upper respiratory tract specimens (nasopharyngeal swab). CDC also recommends testing lower respiratory tract specimens, if available. For patients who develop a productive cough, sputum should be collected and tested for COVID-19. The induction of sputum is not recommended. For patients for whom it is clinically indicated (e.g., those receiving invasive mechanical ventilation), a lower respiratory tract aspirate or bronchoalveolar lavage sample should be collected and tested as a lower respiratory tract specimen. Specimens should be collected as soon as possible once a PUI is identified, regardless of the time of symptom onset. See Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Patients Under Investigation (PUIs) for COVID-19 and Biosafety FAQs for handling and processing specimens from suspected cases and PUIs.
Footnotes
1Fever may be subjective or confirmed
2For healthcare personnel, testing may be considered if there has been exposure to a person with suspected COVID-19 without laboratory confirmation. Because of their often extensive and close contact with vulnerable patients in healthcare settings, even mild signs and symptoms (e.g., sore throat) of COVID-19 should be evaluated among potentially exposed healthcare personnel. Additional information is available in CDC’s Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease 2019 (COVID-19).
3Close contact is defined as—
a) being within approximately 6 feet (2 meters) of a COVID-19 case for a prolonged period of time; close contact can occur while caring for, living with, visiting, or sharing a healthcare waiting area or room with a COVID-19 case
– or –
b) having direct contact with infectious secretions of a COVID-19 case (e.g., being coughed on)
If such contact occurs while not wearing recommended personal protective equipment or PPE (e.g., gowns, gloves, NIOSH-certified disposable N95 respirator, eye protection), criteria for PUI consideration are met.
Additional information is available in CDC’s updated Interim Infection Prevention and Control Recommendations for Patients with Confirmed COVID-19 or Persons Under Investigation for COVID-19 in Healthcare Settings.
Data to inform the definition of close contact are limited. Considerations when assessing close contact include the duration of exposure (e.g., longer exposure time likely increases exposure risk) and the clinical symptoms of the person with COVID-19 (e.g., coughing likely increases exposure risk as does exposure to a severely ill patient). Special consideration should be given to healthcare personnel exposed in healthcare settings as described in CDC’s Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with COVID-19.
4Documentation of laboratory-confirmation of COVID-19 may not be possible for travelers or persons caring for COVID-19 patients in other countries.
5Affected areas are defined as geographic regions where sustained community transmission has been identified. For a list of relevant affected areas, see CDC’s Coronavirus Disease 2019 Information for Travel.
Additional Resources:
State health department after-hours contact listexternal icon
Directory of Local Health Departmentsexternal icon
World Health Organization (WHO) Coronavirusexternal icon
WHO guidance on clinical management of severe acute respiratory infection when COVID-19 is suspectedexternal icon
Content retrieved from: https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria.html.














Add comment